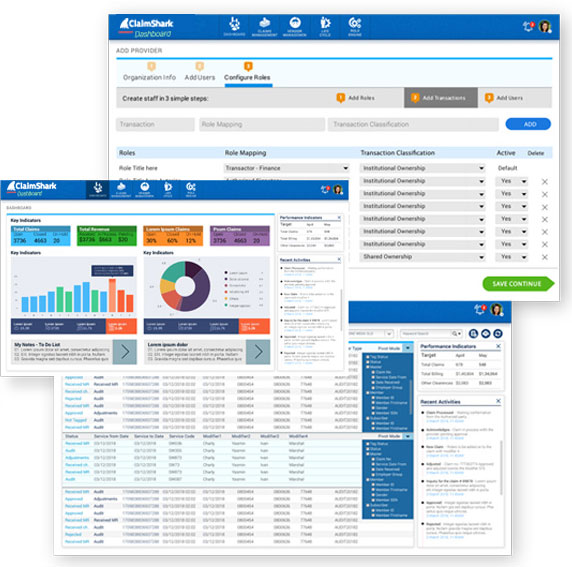
Visibility:
With robust dynamic dashboards that can be customized, Health Plans and vendors get a detailed real time update on the life cycle of the claim, type of recovery by volume and value, plan vs. actual, vendor, provider and more
Dynamic workflow:
Health Plan and vendor can setup their individual workflow queues to manage internal routing and reporting
Productivity:
Vendors get detailed visibility to the productivity of their auditors and collection agents. Vendor details are rolled up, so Health Plans get a comprehensive view of recoveries by vendors, return on investment and value generated.